uses wincrt;
var
A1,A2,A3,A4,A5,Hsl:real;
pilih:char;ket:string[5];
Begin
write('masukkan pilihan nama buah anda:');Readln(pilih);
if pilih='A'then ket:='salak';
if pilih='B'then ket:='nanas';
if pilih='C'then ket:='jambu';
if pilih='D'then ket:='melon';
if pilih='E'then ket:='jeruk';
write(ket);
end.
Rabu, 24 November 2010
Rabu, 10 November 2010
kalkulator sederhana
uses wincrt;var
a1,a2,h:real; plh:integer;
kb:char; label qw;
begin
qw:
writeln;
writeln(' program kalkulator sedehana ');
writeln('++++++++++++++++++++++++++++++');
writeln('1. Program penjumlahan ');
writeln('2. Program pengurangan ');
writeln('3. Program perkalian ');
writeln('4. Program pembagian ');
writeln('==============================');
write('pilih program anda :');readln(plh);
if plh=1 then
begin
write('masukan angka pertama: ');readln(a1);
write('masukan angka kedua : ');readln(a2);
h:=a1+a2;
write('hasilnya adalah : ' ,h:2:0);
end;
if plh=2 then
begin
write('masukan angka pertama: ');readln(a1);
write('masukan angka kedua : ');readln(a2);
h:=a1-a2;
write('hasilnya adalah : ' ,h:2:0);
end;
if plh=3 then
begin
write('masukan angka pertama: ');readln(a1);
write('masukan angka kedua : ');readln(a2);
h:=a1*a2;
write('hasilnya adalah : ' ,h:2:0);
end;
if plh=4 then
begin
write('masukan angka pertama: ');readln(a1);
write('masukan angka kedua : ');readln(a2);
h:=a1*a2;
write('hasilnya adalah : ' ,h:2:0);
end;
writeln;
writeln('+++++++++++++++++++++++++');
writeln('anda mau menjalankan lagi :');
kb:=readkey;
if kb='y' then goto qw;
writeln;
end.
Senin, 25 Oktober 2010
Cinta tak memberikan apa-apa kecuali dirinya sendiri dan tiada mengambil apa pun kecuali dari dirinya sendiri. Cinta tiada memiliki, pun tiada ingin dimiliki; Karena cinta telah cukup bagi cinta.
Cinta berlalu di depan kita, terbalut dalam kerendahan hati; tetapi kita lari dari padanya dalam ketakutan, atau bersembunyi di dalam kegelapan; atau yang lain mengejarnya, untuk berbuat jahat atas namanya.
...pabila cinta memanggilmu... ikutilah dia walau jalannya berliku-liku... Dan, pabila sayapnya merangkummu... pasrahlah serta menyerah, walau pedang tersembunyi di sela sayap itu melukaimu...
...kuhancurkan tulang-tulangku, tetapi aku tidak membuangnya sampai aku mendengar suara cinta memanggilku dan melihat jiwaku siap untuk berpetualang
Tubuh mempunyai keinginan yang tidak kita ketahui. Mereka dipisahkan karena alasan duniawi dan dipisahkan di ujung bumi. Namun jiwa tetap ada di tangan cinta... terus hidup... sampai kematian datang dan menyeret mereka kepada Tuhan...
Jangan menangis, Kekasihku... Janganlah menangis dan berbahagialah, karena kita diikat bersama dalam cinta. Hanya dengan cinta yang indah... kita dapat bertahan terhadap derita kemiskinan, pahitnya kesedihan, dan duka perpisahan
Aku ingin mencintaimu dengan sederhana... seperti kata yang tak sempat diucapkan kayu kepada api yang menjadikannya abu... Aku ingin mencintaimu dengan sederhana... seperti isyarat yang tak sempat dikirimkan awan kepada hujan yang menjadikannya tiada...
Jika cinta tidak dapat mengembalikan engkau kepadaku dalam kehidupan ini... pastilah cinta akan menyatukan kita dalam kehidupan yang akan datang
Apa yang telah kucintai laksana seorang anak kini tak henti-hentinya aku mencintai... Dan, apa yang kucintai kini... akan kucintai sampai akhir hidupku, karena cinta ialah semua yang dapat kucapai... dan tak ada yang akan mencabut diriku dari padanya
Cinta yang dibasuh oleh airmata, akan tetap indah dan suci selamanya.
Manusia tidak dapat menuai cinta sampai dia merasakan perpisahan yang menyedihkan dan yang mampu membuka pikirannya, merasakan kesabaran yang pahit dan kesulitan yang menyedihkan.
Jika kita mencintai seseorang, kita akan senantiasa mendo'akannya walaupun dia tidak berada disisi kita.
Tuhan memberikan kita dua kaki untuk berjalan, dua tangan untuk memegang, dua telinga untuk mendengar dan dua mata untuk melihat. Tetapi mengapa Tuhan hanya menganugerahkan sekeping hati pada kita ? Karena Tuhan telah memberikan sekeping lagi hati pada seseorang untuk kita mencarinya. Itulah Cinta ...
Jangan sesekali mengucapkan selamat tinggal jika kamu masih mau mencoba. Jangan sesekali menyerah jika kamu masih merasa sanggup. Jangan sesekali mengatakan kamu tidak mencintainya lagi, jika kamu masih tidak dapat melupakannya.
Cinta datang kepada orang yang masih mempunyai harapan, walaupun mereka telah dikecewakan. Kepada mereka yang masih percaya, walaupun mereka telah dikhianati. Kepada mereka yang masih ingin mencintai, walaupun mereka telah disakiti sebelumnya dan Kepada mereka yang mempunyai keberanian dan keyakinan untuk membangunkan kembali kepercayaan.
Jangan simpan kata-kata cinta pada orang yang tersayang sehingga dia meninggal dunia lantaran akhirnya kamu terpaksa catatkan kata-kata cinta itu pada pusaranya. Sebaliknya ucapkan kata-kata cinta yang tersimpan dibenakmu itu sekarang selagi ada hayatnya.
Mungkin Tuhan menginginkan kita bertemu dan bercinta dengan orang yang salah sebelum bertemu dengan orang yang tepat, kita harus mengerti bagaimana berterimakasih atas karunia tersebut.
Cinta dapat mengubah pahit menjadi manis, debu beralih emas, keruh menjadi bening, sakit menjadi sembuh, penjara menjadi telaga, derita menjadi nikmat dan kemarahan menjadi rahmat.
Sungguh menyakitkan mencintai seseorang yang tidak mencintaimu, tetapi lebih menyakitkan adalah mencintai seseorang dan kamu tidak pernah memiliki keberanian untuk menyatakan cintamu kepadanya.
Seandainya kamu ingin mencintai atau memiliki hati seorang gadis, ibaratkanlah seperti menyunting sekuntum mawar merah. Kadangkala kamu mencium harum mawar tersebut, tetapi kadangkala kamu terasa bisa duri mawar itu menusuk jari.
Hal yang menyedihkan dalam hidup adalah ketika kamu bertemu seseorang yang sangat berarti bagimu, hanya untuk menemukan bahwa pada akhirnya menjadi tidak berarti dan kamu harus membiarkannya pergi.
Kadangkala kamu tidak menghargai orang yang mencintai kamu sepenuh hati, sehingga kamu kehilangannya. Pada saat itu, tiada guna penyesalan karena perginya tanpa berkata lagi.
Cintailah seseorang itu atas dasar siapa dia sekarang dan bukan siapa dia sebelumnya. Kisah silam tidak perlu diungkit lagi, kiranya kamu benar-benar mencintainya setulus hati.
Hati-hati dengan cinta, karena cinta juga dapat membuat orang sehat menjadi sakit, orang gemuk menjadi kurus, orang normal menjadi gila, orang kaya menjadi miskin, raja menjadi budak, jika cintanya itu disambut oleh para pecinta PALSU.
Kemungkinan apa yang kamu sayangi atau cintai tersimpan keburukan didalamnya dan kemungkinan apa yang kamu benci tersimpan kebaikan didalamnya.
Cinta kepada harta artinya bakhil, cinta kepada perempuan artinya alam, cinta kepada diri artinya bijaksana, cinta kepada mati artinya hidup dan cinta kepada Tuhan artinya Takwa.
Lemparkan seorang yang bahagia dalam bercinta kedalam laut, pasti ia akan membawa seekor ikan. Lemparkan pula seorang yang gagal dalam bercinta ke dalam gudang roti, pasti ia akan mati kelaparan.
Seandainya kamu dapat berbicara dalam semua bahasa manusia dan alam, tetapi tidak mempunyai perasaan cinta dan kasih, dirimu tak ubah seperti gong yang bergaung atau sekedar canang yang gemericing.
Cinta adalah keabadian ... dan kenangan adalah hal terindah yang pernah dimiliki.
Siapapun pandai menghayati cinta, tapi tak seorangpun pandai menilai cinta karena cinta bukanlah suatu objek yang bisa dilihat oleh kasat mata, sebaliknya cinta hanya dapat dirasakan melalui hati dan perasaan.
Cinta mampu melunakkan besi, menghancurkan batu, membangkitkan yang mati dan
meniupkan kehidupan padanya serta membuat budak menjadi pemimpin. Inilah dahsyatnya cinta.
Cinta sebenarnya adalah membiarkan orang yang kamu cintai menjadi dirinya sendiri dan tidak merubahnya menjadi gambaran yang kamu inginkan. Jika tidak, kamu hanya mencintai pantulan diri sendiri yang kamu temukan didalam dirinya.
Kamu tidak akan pernah tahu bila kamu akan jatuh cinta. Namun apabila sampai saatnya itu, raihlah dengan kedua tanganmu dan jangan biarkan dia pergi dengan sejuta rasa tanda tanya dihatinya.
Cinta bukanlah kata murah dan lumrah dituturkan dari mulut kemulut tetapi cinta adalah anugerah Tuhan yang indah dan suci jika manusia dapat menilai kesuciannya.
untuk dicintai juga memang mudah. Tapi untuk dicintai oleh orang yang kita cintai itulah yang sukar diperoleh.
Jika saja kehadiran cinta sekedar untuk mengecewakan, lebih baik cinta itu tak pernah hadir.
Cinta berlalu di depan kita, terbalut dalam kerendahan hati; tetapi kita lari dari padanya dalam ketakutan, atau bersembunyi di dalam kegelapan; atau yang lain mengejarnya, untuk berbuat jahat atas namanya.
...pabila cinta memanggilmu... ikutilah dia walau jalannya berliku-liku... Dan, pabila sayapnya merangkummu... pasrahlah serta menyerah, walau pedang tersembunyi di sela sayap itu melukaimu...
...kuhancurkan tulang-tulangku, tetapi aku tidak membuangnya sampai aku mendengar suara cinta memanggilku dan melihat jiwaku siap untuk berpetualang
Tubuh mempunyai keinginan yang tidak kita ketahui. Mereka dipisahkan karena alasan duniawi dan dipisahkan di ujung bumi. Namun jiwa tetap ada di tangan cinta... terus hidup... sampai kematian datang dan menyeret mereka kepada Tuhan...
Jangan menangis, Kekasihku... Janganlah menangis dan berbahagialah, karena kita diikat bersama dalam cinta. Hanya dengan cinta yang indah... kita dapat bertahan terhadap derita kemiskinan, pahitnya kesedihan, dan duka perpisahan
Aku ingin mencintaimu dengan sederhana... seperti kata yang tak sempat diucapkan kayu kepada api yang menjadikannya abu... Aku ingin mencintaimu dengan sederhana... seperti isyarat yang tak sempat dikirimkan awan kepada hujan yang menjadikannya tiada...
Jika cinta tidak dapat mengembalikan engkau kepadaku dalam kehidupan ini... pastilah cinta akan menyatukan kita dalam kehidupan yang akan datang
Apa yang telah kucintai laksana seorang anak kini tak henti-hentinya aku mencintai... Dan, apa yang kucintai kini... akan kucintai sampai akhir hidupku, karena cinta ialah semua yang dapat kucapai... dan tak ada yang akan mencabut diriku dari padanya
Cinta yang dibasuh oleh airmata, akan tetap indah dan suci selamanya.
Manusia tidak dapat menuai cinta sampai dia merasakan perpisahan yang menyedihkan dan yang mampu membuka pikirannya, merasakan kesabaran yang pahit dan kesulitan yang menyedihkan.
Jika kita mencintai seseorang, kita akan senantiasa mendo'akannya walaupun dia tidak berada disisi kita.
Tuhan memberikan kita dua kaki untuk berjalan, dua tangan untuk memegang, dua telinga untuk mendengar dan dua mata untuk melihat. Tetapi mengapa Tuhan hanya menganugerahkan sekeping hati pada kita ? Karena Tuhan telah memberikan sekeping lagi hati pada seseorang untuk kita mencarinya. Itulah Cinta ...
Jangan sesekali mengucapkan selamat tinggal jika kamu masih mau mencoba. Jangan sesekali menyerah jika kamu masih merasa sanggup. Jangan sesekali mengatakan kamu tidak mencintainya lagi, jika kamu masih tidak dapat melupakannya.
Cinta datang kepada orang yang masih mempunyai harapan, walaupun mereka telah dikecewakan. Kepada mereka yang masih percaya, walaupun mereka telah dikhianati. Kepada mereka yang masih ingin mencintai, walaupun mereka telah disakiti sebelumnya dan Kepada mereka yang mempunyai keberanian dan keyakinan untuk membangunkan kembali kepercayaan.
Jangan simpan kata-kata cinta pada orang yang tersayang sehingga dia meninggal dunia lantaran akhirnya kamu terpaksa catatkan kata-kata cinta itu pada pusaranya. Sebaliknya ucapkan kata-kata cinta yang tersimpan dibenakmu itu sekarang selagi ada hayatnya.
Mungkin Tuhan menginginkan kita bertemu dan bercinta dengan orang yang salah sebelum bertemu dengan orang yang tepat, kita harus mengerti bagaimana berterimakasih atas karunia tersebut.
Cinta dapat mengubah pahit menjadi manis, debu beralih emas, keruh menjadi bening, sakit menjadi sembuh, penjara menjadi telaga, derita menjadi nikmat dan kemarahan menjadi rahmat.
Sungguh menyakitkan mencintai seseorang yang tidak mencintaimu, tetapi lebih menyakitkan adalah mencintai seseorang dan kamu tidak pernah memiliki keberanian untuk menyatakan cintamu kepadanya.
Seandainya kamu ingin mencintai atau memiliki hati seorang gadis, ibaratkanlah seperti menyunting sekuntum mawar merah. Kadangkala kamu mencium harum mawar tersebut, tetapi kadangkala kamu terasa bisa duri mawar itu menusuk jari.
Hal yang menyedihkan dalam hidup adalah ketika kamu bertemu seseorang yang sangat berarti bagimu, hanya untuk menemukan bahwa pada akhirnya menjadi tidak berarti dan kamu harus membiarkannya pergi.
Kadangkala kamu tidak menghargai orang yang mencintai kamu sepenuh hati, sehingga kamu kehilangannya. Pada saat itu, tiada guna penyesalan karena perginya tanpa berkata lagi.
Cintailah seseorang itu atas dasar siapa dia sekarang dan bukan siapa dia sebelumnya. Kisah silam tidak perlu diungkit lagi, kiranya kamu benar-benar mencintainya setulus hati.
Hati-hati dengan cinta, karena cinta juga dapat membuat orang sehat menjadi sakit, orang gemuk menjadi kurus, orang normal menjadi gila, orang kaya menjadi miskin, raja menjadi budak, jika cintanya itu disambut oleh para pecinta PALSU.
Kemungkinan apa yang kamu sayangi atau cintai tersimpan keburukan didalamnya dan kemungkinan apa yang kamu benci tersimpan kebaikan didalamnya.
Cinta kepada harta artinya bakhil, cinta kepada perempuan artinya alam, cinta kepada diri artinya bijaksana, cinta kepada mati artinya hidup dan cinta kepada Tuhan artinya Takwa.
Lemparkan seorang yang bahagia dalam bercinta kedalam laut, pasti ia akan membawa seekor ikan. Lemparkan pula seorang yang gagal dalam bercinta ke dalam gudang roti, pasti ia akan mati kelaparan.
Seandainya kamu dapat berbicara dalam semua bahasa manusia dan alam, tetapi tidak mempunyai perasaan cinta dan kasih, dirimu tak ubah seperti gong yang bergaung atau sekedar canang yang gemericing.
Cinta adalah keabadian ... dan kenangan adalah hal terindah yang pernah dimiliki.
Siapapun pandai menghayati cinta, tapi tak seorangpun pandai menilai cinta karena cinta bukanlah suatu objek yang bisa dilihat oleh kasat mata, sebaliknya cinta hanya dapat dirasakan melalui hati dan perasaan.
Cinta mampu melunakkan besi, menghancurkan batu, membangkitkan yang mati dan
meniupkan kehidupan padanya serta membuat budak menjadi pemimpin. Inilah dahsyatnya cinta.
Cinta sebenarnya adalah membiarkan orang yang kamu cintai menjadi dirinya sendiri dan tidak merubahnya menjadi gambaran yang kamu inginkan. Jika tidak, kamu hanya mencintai pantulan diri sendiri yang kamu temukan didalam dirinya.
Kamu tidak akan pernah tahu bila kamu akan jatuh cinta. Namun apabila sampai saatnya itu, raihlah dengan kedua tanganmu dan jangan biarkan dia pergi dengan sejuta rasa tanda tanya dihatinya.
Cinta bukanlah kata murah dan lumrah dituturkan dari mulut kemulut tetapi cinta adalah anugerah Tuhan yang indah dan suci jika manusia dapat menilai kesuciannya.
untuk dicintai juga memang mudah. Tapi untuk dicintai oleh orang yang kita cintai itulah yang sukar diperoleh.
Jika saja kehadiran cinta sekedar untuk mengecewakan, lebih baik cinta itu tak pernah hadir.
Minggu, 17 Oktober 2010
"....Aku sangat menggaguminya,
Bahkan aku gila dibuat,nya.
senyumnya yang manis dan tatapan matanya yang tajam membuatku gila..
oh ,,Tuhan tolong aku melupakannya dari otakku ini,,,
aku tahu ada seseorang yang lebih menyayanginya daripada aku,,
apakah ini namaya cinta atau apa kekaguman saja pada kelebihannya?...." harapan gadis bermata bulat dalam hatinya...
Waktu berjalan sesukanya, mengalir kemana ia mau, ia suka dan ia inginkan.Kini perasan itu hilang bersamanya.Tak ada lagi dan tak mau lagi.
Hujan.Hemmm....hujan.Ya hujan,dan memang betul hujan kali ini.Aku senang, senang dan senang.Memang waktu tak lagi pagi.Matahari pun sudah undur dari pos jaganya yang membosankan.Dan tugasnya telah usai ia kerjakan kali ini dengan baik.bahkan sangat baik.
Gadis pun pulang dengan bahagianya ia,karena kali ini ia bisa menatap mata itu lagi tepat di depanya dengan jelas sejelas ia mengeja kata "love" yang sehari hari ia gumamkan lewat mulut kecilnya. "Love" banyak orang memanggil dan menyebut namnya "love si anak mama".Ia pun jengkel dan muak jika orang menyebut nama itu.Namun apa boleh buat nama itu adalah nama terindah yang ia terima dari orang yang sangat ia sayangi.
Tak disangka triakan harimau itu datang lagi. keras dan makin keras kali ini terdengar di telinganya.
"Tunguuuuuuuuuuu aku lov.....!!!!!" kata bunga dengan bertenaga.
love menoleh dengan perlahan ia melihatnya.
"Bukkkkkg....." tangannya yang besar tepat di pundaknya.
Lalu.....
Bahkan aku gila dibuat,nya.
senyumnya yang manis dan tatapan matanya yang tajam membuatku gila..
oh ,,Tuhan tolong aku melupakannya dari otakku ini,,,
aku tahu ada seseorang yang lebih menyayanginya daripada aku,,
apakah ini namaya cinta atau apa kekaguman saja pada kelebihannya?...." harapan gadis bermata bulat dalam hatinya...
Waktu berjalan sesukanya, mengalir kemana ia mau, ia suka dan ia inginkan.Kini perasan itu hilang bersamanya.Tak ada lagi dan tak mau lagi.
Hujan.Hemmm....hujan.Ya hujan,dan memang betul hujan kali ini.Aku senang, senang dan senang.Memang waktu tak lagi pagi.Matahari pun sudah undur dari pos jaganya yang membosankan.Dan tugasnya telah usai ia kerjakan kali ini dengan baik.bahkan sangat baik.
Gadis pun pulang dengan bahagianya ia,karena kali ini ia bisa menatap mata itu lagi tepat di depanya dengan jelas sejelas ia mengeja kata "love" yang sehari hari ia gumamkan lewat mulut kecilnya. "Love" banyak orang memanggil dan menyebut namnya "love si anak mama".Ia pun jengkel dan muak jika orang menyebut nama itu.Namun apa boleh buat nama itu adalah nama terindah yang ia terima dari orang yang sangat ia sayangi.
Tak disangka triakan harimau itu datang lagi. keras dan makin keras kali ini terdengar di telinganya.
"Tunguuuuuuuuuuu aku lov.....!!!!!" kata bunga dengan bertenaga.
love menoleh dengan perlahan ia melihatnya.
"Bukkkkkg....." tangannya yang besar tepat di pundaknya.
Lalu.....
Tuhan memberi kita dua kaki untuk berjalan, dua tangan untuk memegang, dua telinga untuk mendengar dan dua mata untuk melihat. Tetapi mengapa Tuhan hanya menganugerahkan sekeping hati pada kita? Karena Tuhan telah memberikan sekeping lagi hati pada seseorang untuk kita mencarinya. Itulah namanya Cinta.
Jangan sesekali mengucapkan selamat tinggal jika kamu masih mau mencoba. Jangan sesekali menyerah jika kamu masih merasa sanggup. Jangan sesekali mengatakan kamu tidak mencintainya lagi jika kamu masih tidak dapat melupakannya.
Jangan sesekali mengucapkan selamat tinggal jika kamu masih mau mencoba. Jangan sesekali menyerah jika kamu masih merasa sanggup. Jangan sesekali mengatakan kamu tidak mencintainya lagi jika kamu masih tidak dapat melupakannya.
Rabu, 13 Oktober 2010
poem corner
Hargai Milikmu
Hargailah segala yang kau miliki; anda akan memiliki lebih lagi. Jika anda fokus pada apa yang tidak anda miliki, anda tidak akan pernah merasa cukup dalam hal apapun.Be thankful for what you have; you’ll end up having more. If you concentrate on what you don’t have, you will never, ever have enough.
~ Oprah Winfrey
Kamis, 30 September 2010
puisi chairil anwar
AKU
Kalau sampai waktuku
'Ku mau tak seorang kan merayu
Tidak juga kau
Tak perlu sedu sedan itu
Aku ini binatang jalang
Dari kumpulannya terbuang
Biar peluru menembus kulitku
Aku tetap meradang menerjang
Luka dan bisa kubawa berlari
Berlari
Hingga hilang pedih peri
Dan aku akan lebih tidak perduli
Aku mau hidup seribu tahun lagi
Maret 1943
Kalau sampai waktuku
'Ku mau tak seorang kan merayu
Tidak juga kau
Tak perlu sedu sedan itu
Aku ini binatang jalang
Dari kumpulannya terbuang
Biar peluru menembus kulitku
Aku tetap meradang menerjang
Luka dan bisa kubawa berlari
Berlari
Hingga hilang pedih peri
Dan aku akan lebih tidak perduli
Aku mau hidup seribu tahun lagi
Maret 1943
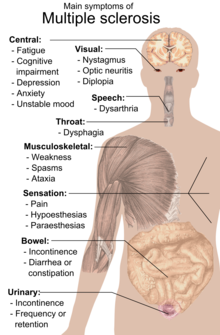
Multiple sclerosis
Multiple sclerosis
From Wikipedia, the free encyclopedia
Jump to: navigation, search
| Multiple sclerosis | |
|---|---|
| Classification and external resources | |
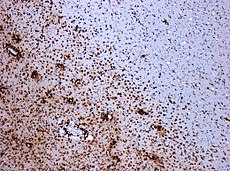 Demyelinization by MS. The CD68 colored tissue shows several macrophages in the area of the lesion. Original scale 1:100 | |
| ICD-10 | G35. |
| ICD-9 | 340 |
| OMIM | 126200 |
| DiseasesDB | 8412 |
| MedlinePlus | 000737 |
| eMedicine | neuro/228 oph/179 emerg/321 pmr/82 radio/461 |
| MeSH | D009103 |
MS affects the ability of nerve cells in the brain and spinal cord to communicate with each other. Nerve cells communicate by sending electrical signals called action potentials down long fibers called axons, which are wrapped in an insulating substance called myelin. In MS, the body's own immune system attacks and damages the myelin. When myelin is lost, the axons can no longer effectively conduct signals.[4] The name multiple sclerosis refers to scars (scleroses—better known as plaques or lesions) particularly in the white matter of the brain and spinal cord, which is mainly composed of myelin.[3] Although much is known about the mechanisms involved in the disease process, the cause remains unknown. Theories include genetics or infections. Different environmental risk factors have also been found.[4][5]
Almost any neurological symptom can appear with the disease, and often progresses to physical and cognitive disability.[4] MS takes several forms, with new symptoms occurring either in discrete attacks (relapsing forms) or slowly accumulating over time (progressive forms).[6] Between attacks, symptoms may go away completely, but permanent neurological problems often occur, especially as the disease advances.[6]
There is no known cure for MS. Treatments attempt to return function after an attack, prevent new attacks, and prevent disability.[4] MS medications can have adverse effects or be poorly tolerated, and many patients pursue alternative treatments, despite the lack of supporting scientific study. The prognosis is difficult to predict; it depends on the subtype of the disease, the individual patient's disease characteristics, the initial symptoms and the degree of disability the person experiences as time advances.[7] Life expectancy of patients is 5 to 10 years lower to that of the unaffected population.[1]
Classification
Several subtypes, or patterns of progression, have been described. Subtypes use the past course of the disease in an attempt to predict the future course. They are important not only for prognosis but also for therapeutic decisions. In 1996 the United States National Multiple Sclerosis Society standardized four subtype definitions:[6]- relapsing remitting,
- secondary progressive,
- primary progressive, and
- progressive relapsing.
Secondary progressive MS (sometimes called "galloping MS") describes around 65 % of those with an initial relapsing-remitting MS, who then begin to have progressive neurologic decline between acute attacks without any definite periods of remission.[1][6] Occasional relapses and minor remissions may appear.[6] The median time between disease onset and conversion from relapsing-remitting to secondary progressive MS is 19 years.[10]
The primary progressive subtype describes the approximately 10–15% of individuals who never have remission after their initial MS symptoms.[11] It is characterized by progression of disability from onset, with no, or only occasional and minor, remissions and improvements.[6] The age of onset for the primary progressive subtype is later than for the relapsing-remitting, but similar to mean age of progression between the relapsing-remitting and the secondary progressive. In both cases it is around 40 years of age.[1]
Progressive relapsing MS describes those individuals who, from onset, have a steady neurologic decline but also suffer clear superimposed attacks. This is the least common of all subtypes.[6]
Atypical variants of MS with non-standard behavior have been described; these include Devic's disease, Balo concentric sclerosis, Schilder's diffuse sclerosis and Marburg multiple sclerosis. There is debate on whether they are MS variants or different diseases.[12] Multiple sclerosis also behaves differently in children, taking more time to reach the progressive stage.[1] Nevertheless they still reach it at a lower mean age than adults.[1]
[edit] Signs and symptoms
Main article: Multiple sclerosis signs and symptoms
The person with MS can suffer almost any neurological symptom or sign, including changes in sensation such as loss of sensitivity or tingling, pricking or numbness (hypoesthesia and paraesthesia), muscle weakness, muscle spasms, or difficulty in moving; difficulties with coordination and balance (ataxia); problems in speech (dysarthria) or swallowing (dysphagia), visual problems (nystagmus, optic neuritis including phosphenes,[13][14] or diplopia), fatigue, acute or chronic pain, and bladder and bowel difficulties.[1] Cognitive impairment of varying degrees and emotional symptoms of depression or unstable mood are also common.[1] Uhthoff's phenomenon, an exacerbation of extant symptoms due to an exposure to higher than usual ambient temperatures, and Lhermitte's sign, an electrical sensation that runs down the back when bending the neck, are particularly characteristic of MS although not specific.[1] The main clinical measure of disability progression and symptom severity is the Expanded Disability Status Scale or EDSS.[15]Symptoms of MS usually appear in episodic acute periods of worsening (called relapses, exacerbations, bouts, attacks, or "flare-ups"), in a gradually progressive deterioration of neurologic function, or in a combination of both.[6] Multiple sclerosis relapses are often unpredictable, occurring without warning and without obvious inciting factors with a rate rarely above 1 and a half per year.[1] Some attacks, however, are preceded by common triggers. Relapses occur more frequently during spring and summer.[16] Viral infections such as the common cold, influenza, or gastroenteritis increase the risk of relapse.[1] Stress may also trigger an attack.[17] Pregnancy affects the susceptibility to relapse, with a lower relapse rate at each trimester of gestation. During the first few months after delivery, however, the risk of relapse is increased.[1] Overall, pregnancy does not seem to influence long-term disability. Many potential triggers have been examined and found not to influence MS relapse rates. There is no evidence that vaccination and breast feeding,[1] physical trauma,[18] or Uhthoff's phenomenon[16] are relapse triggers.
[edit] Causes
Most likely MS occurs as a result of some combination of genetic, environmental and infectious factors.[1] Epidemiological studies of MS have provided hints on possible causes for the disease. Theories try to combine the known data into plausible explanations, but none has proved definitive.[edit] Genetics
MS is not considered a hereditary disease. However, a number of genetic variations have been shown to increase the risk of developing the disease.[19]The risk of acquiring MS is higher in relatives of a person with the disease than in the general population, especially in the case of siblings, parents, and children.[4] The disease has an overall familial recurrence rate of 20%.[1] In the case of monozygotic twins, concordance occurs only in about 35% of cases, while it goes down to around 5% in the case of siblings and even lower in half-siblings. This indicates susceptibility is partly polygenically driven.[1][4]
It seems to be more common in some ethnic groups than others.
Apart from familial studies, specific genes have been linked with MS. Differences in the human leukocyte antigen (HLA) system—a group of genes in chromosome 6 that serves as the major histocompatibility complex (MHC) in humans—increase the probability of suffering MS.[1] The most consistent finding is the association between multiple sclerosis and alleles of the MHC defined as DR15 and DQ6.[1] Other loci have shown a protective effect, such as HLA-C554 and HLA-DRB1*11.[1]
[edit] Environmental factors
Different environmental factors, both of infectious and non infectious origin have been proposed as risk factors for MS. Although some are partly modifiable, only further research—especially clinical trials—will reveal whether their elimination can help prevent MS.[20]MS is more common in people who live farther from the equator, although many exceptions exist.[1] Decreased sunlight exposure has been linked with a higher risk of MS.[20] Decreased vitamin D production and intake has been the main biological mechanism used to explain the higher risk among those less exposed to sun.[20][21][22]
Severe stress may also be a risk factor although evidence is weak.[20] Smoking has also been shown to be an independent risk factor for developing MS.[21] Association with occupational exposures and toxins—mainly solvents—has been evaluated, but no clear conclusions have been reached.[20] Vaccinations were also considered as causal factors for the disease; however, most studies show no association between MS and vaccines.[20] Several other possible risk factors, such as diet and hormone intake, have been investigated; however, more evidence is needed to confirm or refute their relation with the disease.[21]
Gout occurs less than would statistically be expected in people with MS, and low levels of uric acid have been found in MS patients as compared to normal individuals. This led to the theory that uric acid protects against MS, although its exact importance remains unknown.[23]
[edit] Infections
Many microbes have been proposed as potential infectious triggers of MS, but none has been substantiated.[4]Genetic susceptibility can explain some of the geographic and epidemiological variations in MS incidence, like the high incidence of the disease among some families or the risk decline with genetic distance, but does not account for other phenomena, such as the changes in risk that occur with migration at an early age.[5] An explanation for this epidemiological finding could be that some kind of infection, produced by a widespread microbe rather than a rare pathogen, is the origin of the disease.[5] Different hypotheses have elaborated on the mechanism by which this may occur. The hygiene hypothesis proposes that exposure to several infectious agents early in life is protective against MS, the disease being a response to a later encounter with such agents.[1] The prevalence hypothesis proposes that the disease is due to a pathogen more common in regions of high MS prevalence. This pathogen is very common, causing in most individuals an asymptomatic persistent infection. Only in a few cases, and after many years since the original infection, does it cause demyelination.[5][24] The hygiene hypothesis has received more support than the prevalence hypothesis.[5]
Evidence for viruses as a cause includes the presence of oligoclonal bands in the brain and cerebrospinal fluid of most patients, the association of several viruses with human demyelination encephalomyelitis, and induction of demyelination in animals through viral infection.[25] Human herpes viruses are a candidate group of viruses linked to MS. Individuals who have never been infected by the Epstein-Barr virus have a reduced risk of having the disease, and those infected as young adults have a greater risk than those who had it at a younger age.[1][5] Although some consider that this goes against the hygiene hypothesis, since the non-infected have probably experienced a more hygienic upbringing,[5] others believe that there is no contradiction since it is a first encounter at a later moment with the causative virus that is the trigger for the disease.[1] Other diseases that have also been related with MS are measles, mumps and rubella.[1]
[edit] Pathophysiology
Main article: Pathophysiology of multiple sclerosis
[edit] Blood-brain barrier breakdown
[edit] Autoimmunology
MS is currently believed to be an immune-mediated disorder mediated by a complex interaction of the individual's genetics and as yet unidentified environmental insults.[4] Damage is believed to be caused by the patient's own immune system. The immune system attacks the nervous system, possibly as a result of exposure to a molecule with a similar structure to one of its own.[4]- Lesions
More specifically, MS destroys oligodendrocytes, the cells responsible for creating and maintaining a fatty layer—known as the myelin sheath—which helps the neurons carry electrical signals.[4] MS results in a thinning or complete loss of myelin and, as the disease advances, the cutting (transection) of the neuron's extensions or axons. When the myelin is lost, a neuron can no longer effectively conduct electrical signals.[4] A repair process, called remyelination, takes place in early phases of the disease, but the oligodendrocytes cannot completely rebuild the cell's myelin sheath.[26] Repeated attacks lead to successively fewer effective remyelinations, until a scar-like plaque is built up around the damaged axons.[26] Different lesion patterns have been described.[27]
- Inflammation
The T cells recognize myelin as foreign and attack it as if it were an invading virus. This triggers inflammatory processes, stimulating other immune cells and soluble factors like cytokines and antibodies. Leaks form in the blood–brain barrier, which in turn cause a number of other damaging effects such as swelling, activation of macrophages, and more activation of cytokines and other destructive proteins.[4]
[edit] Diagnosis

T1-weighted MRI scans (post-contrast) of the same brain slice at monthly intervals. Bright spots indicate active lesions.
Clinical data alone may be sufficient for a diagnosis of MS if an individual has suffered separate episodes of neurologic symptoms characteristic of MS.[31] Since some people seek medical attention after only one attack, other testing may hasten and ease the diagnosis. The most commonly used diagnostic tools are neuroimaging, analysis of cerebrospinal fluid and evoked potentials. Magnetic resonance imaging of the brain and spine shows areas of demyelination (lesions or plaques). Gadolinium can be administered intravenously as a contrast to highlight active plaques and, by elimination, demonstrate the existence of historical lesions not associated with symptoms at the moment of the evaluation.[31][33] Testing of cerebrospinal fluid obtained from a lumbar puncture can provide evidence of chronic inflammation of the central nervous system. The cerebrospinal fluid is tested for oligoclonal bands of IgG on electrophoresis, which are an inflammation marker found in 75–85% of people with MS.[31][34] The nervous system of a person with MS responds less actively to stimulation of the optic nerve and sensory nerves due to demyelination of such pathways. These brain responses can be examined using visual and sensory evoked potentials.[35]
[edit] Management
Main article: Treatment of multiple sclerosis
Although there is no known cure for multiple sclerosis, several therapies have proven helpful. The primary aims of therapy are returning function after an attack, preventing new attacks, and preventing disability. As with any medical treatment, medications used in the management of MS have several adverse effects. Alternative treatments are pursued by some patients, despite the shortage of supporting, comparable, replicated scientific study.[edit] Acute attacks
During symptomatic attacks, administration of high doses of intravenous corticosteroids, such as methylprednisolone, is the routine therapy for acute relapses.[1] Although generally effective in the short term for relieving symptoms, corticosteroid treatments do not appear to have a significant impact on long-term recovery.[36] Oral and intravenous administration seem to have similar efficacy.[37] Consequences of severe attacks which do not respond to corticosteroids might be treated by plasmapheresis.[1][edit] Disease-modifying treatments
All five kinds of medications are modestly effective at decreasing the number of attacks in relapsing-remitting MS (RRMS) while the capacity of interferons and glatiramer acetate is more controversial. Studies of their long-term effects are still lacking.[1][38] Comparisons between immunomodulators (all but mitoxantrone) show that the most effective is natalizumab, both in terms of relapse rate reduction and halting disability progression.[39] Mitoxantrone may be the most effective of them all; however, it is generally not considered as a long-term therapy, as its use is limited by severe secondary effects.[1][38] The earliest clinical presentation of RRMS is the clinically isolated syndrome (CIS). Treatment with interferons during an initial attack can decrease the chance that a patient will develop clinical MS.[1]
Treatment of progressive MS is more difficult than relapsing-remitting MS. Mitoxantrone has shown positive effects in patients with secondary progressive and progressive relapsing courses. It is moderately effective in reducing the progression of the disease and the frequency of relapses in patients in short-term follow-up.[40] No treatment has been proven to modify the course of primary progressive MS.[41]
As with many medical treatments, these treatments have several adverse effects. One of the most common is irritation at the injection site for glatiramer acetate and the interferon treatments. Over time, a visible dent at the injection site, due to the local destruction of fat tissue, known as lipoatrophy, may develop. Interferons produce symptoms similar to influenza;[42] some patients taking glatiramer experience a post-injection reaction manifested by flushing, chest tightness, heart palpitations, breathlessness, and anxiety, which usually lasts less than thirty minutes.[43] More dangerous but much less common are liver damage from interferons,[44] severe cardiotoxicity, infertility, and acute myeloid leukaemia of mitoxantrone,[1][38] and the putative link between natalizumab and some cases of progressive multifocal leukoencephalopathy.[1]
[edit] Management of the effects of MS
Disease-modifying treatments reduce the progression rate of the disease, but do not stop it. As multiple sclerosis progresses, the symptomatology tends to increase. The disease is associated with a variety of symptoms and functional deficits that result in a range of progressive impairments and disability. Management of these deficits is therefore very important. Both drug therapy and neurorehabilitation have shown to ease the burden of some symptoms, though neither influences disease progression.[1][45] Some symptoms have a good response to medication, such as unstable bladder and spasticity, while management of many others is much more complicated.[1] As for any patient with neurologic deficits, a multidisciplinary approach is key to improving quality of life; however, there are particular difficulties in specifying a ‘core team’ because people with MS may need help from almost any health profession or service at some point.[1] Multidisciplinary rehabilitation programmes increase activity and participation of patients but do not influence impairment level.[46][edit] Alternative treatments
As with most chronic diseases, alternative treatments are pursued by some patients, despite the shortage of supporting, comparable, replicated scientific study.[47] Examples are dietary regimens,[48] herbal medicine, including the use of medical cannabis,[49] hyperbaric oxygenation[50] and self-infection with hookworm.[51][edit] Prognosis

Disability-adjusted life year for multiple sclerosis per 100,000 inhabitants in 2004
no data less than 13 13–16 16–19 19–22 22–25 25–28 28–31 31–34 34–37 37–40 40–43 more than 43
Female sex, relapsing-remitting subtype, optic neuritis or sensory symptoms at onset, few attacks in the initial years and especially early age at onset, are associated with a better course.[7][52]
The life expectancy of people with MS is 5 to 10 years lower than that of unaffected people.[1] Almost 40% of patients reach the seventh decade of life.[52] Nevertheless, two thirds of the deaths in people with MS are directly related to the consequences of the disease.[1] Suicide is also a much more important risk of death than in the healthy population, while infections and complications are especially hazardous for the more disabled ones.[1]
Although most patients lose the ability to walk prior to death, 90% are still capable of independent walking at 10 years from onset, and 75% at 15 years.[52][53]
[edit] Epidemiology
Two main measures are used in epidemiological studies: incidence and prevalence. Incidence is the number of new cases per unit of person–time at risk (usually number of new cases per thousand person–years); while prevalence is the total number of cases of the disease in the population at a given time. Prevalence is known to depend not only on incidence, but also on survival rate and migrations of affected people. MS has a prevalence that ranges between 2 and 150 per 100,000 depending on the country or specific population.[2] Studies on populational and geographical patterns of epidemiological measures have been very common in MS,[24] and have led to the proposal of different etiological (causal) theories.[5][20][21][24]MS usually appears in adults in their thirties but it can also appear in children.[1] The primary progressive subtype is more common in people in their fifties.[11] As with many autoimmune disorders, the disease is more common in women, and the trend may be increasing.[1][54] In children, the sex ratio difference is higher,[1] while in people over fifty, MS affects males and females almost equally.[11]
There is a north-to-south gradient in the northern hemisphere and a south-to-north gradient in the southern hemisphere, with MS being much less common in people living near the equator.[1][54] Climate, sunlight and intake of vitamin D have been investigated as possible causes of the disease that could explain this latitude gradient.[21] However, there are important exceptions to the north-south pattern and changes in prevalence rates over time;[1] in general, this trend might be disappearing.[54] This indicates that other factors such as environment or genetics have to be taken into account to explain the origin of MS.[1] MS is also more common in regions with northern Europe populations.[1] But even in regions where MS is common, some ethnic groups are at low risk of developing the disease, including the Samis, Turkmen, Amerindians, Canadian Hutterites, Africans, and New Zealand Māori.[20]
Environmental factors during childhood may play an important role in the development of MS later in life. Several studies of migrants show that if migration occurs before the age of 15, the migrant acquires the new region's susceptibility to MS. If migration takes place after age 15, the migrant retains the susceptibility of his home country.[1][20] However, the age–geographical risk for developing multiple sclerosis may span a larger timescale.[1] A relationship between season of birth and MS has also been found which lends support to an association with sunlight and vitamin D. For example fewer people with MS are born in November as compared to May.[55]
[edit] History
[edit] Medical discovery
The French neurologist Jean-Martin Charcot (1825–1893) was the first person to recognize multiple sclerosis as a distinct disease in 1868.[56] Summarizing previous reports and adding his own clinical and pathological observations, Charcot called the disease sclerose en plaques. The three signs of MS now known as Charcot's triad 1 are nystagmus, intention tremor, and telegraphic speech, though these are not unique to MS. Charcot also observed cognition changes, describing his patients as having a "marked enfeeblement of the memory" and "conceptions that formed slowly".[3]Prior to Charcot, Robert Carswell (1793–1857), a British professor of pathology, and Jean Cruveilhier (1791–1873), a French professor of pathologic anatomy, had described and illustrated many of the disease's clinical details, but did not identify it as a separate disease.[56] Specifically, Carswell described the injuries he found as "a remarkable lesion of the spinal cord accompanied with atrophy".[1] Under the microscope, Swiss pathologist Georg Eduard Rindfleisch (1836-1908) noted in 1863 that the inflammation-associated lesions were distributed around veins.[57][58]
After Charcot's description, Eugène Devic (1858–1930), Jozsef Balo (1895–1979), Paul Ferdinand Schilder (1886–1940), and Otto Marburg (1874–1948) described special cases of the disease. During all the 20th century there was an important development on the theories about the cause and pathogenesis of MS while efficacious treatments began to appear in 1990.[1]
[edit] Historical cases
There are several historical accounts of people who lived before or shortly after the disease was described by Charcot and probably had MS.A young woman called Halldora, who lived in Iceland around the year 1200, suddenly lost her vision and mobility, but after praying to the saints, recovered them seven days after. Saint Lidwina of Schiedam (1380–1433), a Dutch nun, may be one of the first clearly identifiable MS patients. From the age of 16 until her death at 53, she suffered intermittent pain, weakness of the legs, and vision loss—symptoms typical of MS.[59] Both cases have led to the proposal of a 'Viking gene' hypothesis for the dissemination of the disease.[60]
Augustus Frederick d'Este (1794-1848), son of Prince Augustus Frederick, Duke of Sussex and Lady Augusta Murray and the grandson of George III of the United Kingdom, almost certainly suffered from MS. D'Este left a detailed diary describing his 22 years living with the disease. His diary began in 1822 and ended in 1846, although it remained unknown until 1948. His symptoms began at age 28 with a sudden transient visual loss after the funeral of a friend. During the course of his disease, he developed weakness of the legs, clumsiness of the hands, numbness, dizziness, bladder disturbances, and erectile dysfunction. In 1844, he began to use a wheelchair. Despite his illness, he kept an optimistic view of life.[61][62]
Another early account of MS was kept by the British diarist W. N. P. Barbellion, nom-de-plume of Bruce Frederick Cummings (1889-1919), who maintained a detailed log of his diagnosis and struggle with MS.[62] His diary was published in 1919 as The Journal of a Disappointed Man.[63]
[edit] Research directions
Main article: Therapies under investigation for multiple sclerosis
[edit] Therapies

Chemical structure of alemtuzumab
In 2010, an FDA committee recommended approving fingolimod for the treatment of MS attacks,[65] and on September 22, 2010, fingolimod (trade name Gilenia) became the first oral drug approved by the Food and Drug Administration to reduce relapses and delay disability progression in patients with relapsing forms of multiple sclerosis.[66] Clinical trials of fingolimod have demonstrated side effects in treated patients, including cardiovascular conditions, macular edema, infections, liver toxicity and malignancies.[67][68]
Much interest has been focussed on the prospect of utilizing vitamin D analogs in the prevention and management of CIS and MS, especially given its possible role in the pathogenesis of the disease. While there is anecdotal evidence of benefit for low dose naltrexone,[69] only results from a pilot study in primary progressive MS have been published.[70]
[edit] Disease biomarkers
The variable clinical presentation of MS and the lack of diagnostic laboratory tests lead to delays in diagnosis and the impossibility of predicting diagnosis. New diagnostic methods are being investigated. These include work with anti-myelin antibodies, analysis of microarray gene expression and studies with serum and cerebrospinal fluid but none of them has yielded reliable positive results.[71]Currently there are no clinically established laboratory investigations available that can predict prognosis. However, several promising approaches have been proposed. Investigations on the prediction of evolution have centred on monitoring disease activity. Disease activation biomarkers include interleukin-6, nitric oxide and nitric oxide synthase, osteopontin, and fetuin-A.[71] On the other hand since disease progression is the result of neurodegeneration the roles of proteins indicative of neuronal, axonal, and glial loss such as neurofilaments, tau and N-acetylaspartate are under investigation.[71]
A final investigative field is work with biomarkers that distinguish between medication responders and nonresponders.[71]
[edit] Chronic cerebrospinal venous insufficiency
Main article: Chronic cerebrospinal venous insufficiency
Vascular surgeon Paolo Zamboni has conducted research suggesting that MS involves a vascular disease process he refers to as chronic cerebrospinal venous insufficiency (CCSVI, CCVI), in which veins from the brain are constricted. He found what he believes to be CCSVI in the majority of MS patients, performed a surgical procedure to correct it and claims that 73% of patients improved.[72] However, the surgeries were neither controlled nor randomized. The neurology community currently recommends not to use the proposed treatment until its effectiveness is confirmed by controlled studies, the need for which has been recognized by the scientific bodies engaged in MS research.[73]
Langganan:
Postingan (Atom)